Home Innovation Robotics How is robotics used in health...
How is robotics used in healthcare, and what are its benefits?
Robotics

Business Fortune
20 September, 2024
Throughout history, robots have been employed in a variety of fields, such as manufacturing, construction, and military operations. But their application to medicine is still relatively recent. With the daily introduction of new technologies and methods, the medical industry is always changing. Due to the advantages that robots offer to both doctors and patients, their usage in surgery has increased recently.
How is robotics used in healthcare, and what are its benefits?
By enabling high-quality patient care, optimizing clinical procedures, and fostering a safer patient environment, the integration of robotics in healthcare has completely transformed the sector.
In research labs, robotics and robotization are utilized to automate labor-intensive, repetitive, and manual processes. It allows scientists and professionals to focus on more research that will lead to quicker breakthroughs.
Hospitals and training facilities have been using medical robots to carry out a variety of jobs to reduce the possibility of pathogen exposure during the COVID-19 pandemic.
-
High standards of patient care robots: Efficient clinical procedures and a secure environment for both patients and healthcare staff are all made possible by the use of robotics-assisted therapy in healthcare.
-
Superior Patient Treatment: Medical robots enable minimally invasive treatments, regular and tailored surveillance for patient care robots with long-term conditions, intelligent treatments, and social interaction for elderly patients.
-
Simplified Clinical Processes: Autonomous mobile robots (AMRs) guarantee further compatible processes, lessen the physical burden on human workers, and simplify repetitive jobs. By monitoring medication inventory and putting it in the right stores, these robots can help with staff needs and difficulties.
-
Safe Work Environment: In hospitals where disease exposure poses a risk, AMRs convey supplies and linens to help keeping healthcare personnel safe. Robots for heavy lifting, cleaning, and disinfection can lower hospital-acquired infections (HAIs) by limiting pathogen exposure.
Innovations in Robotic Technology for Healthcare
Another fascinating breakthrough in healthcare precision medicine robotics is the creation of Nano robots. These small robots have potential use in targeted administration of drugs, precise tissue healing, and molecular early disease detection. This breakthrough opens the door for revolutionary therapeutic approaches and precision medicine robotics.
Key Benefits of Robotics in Healthcare
Numerous advantages exist for robotics in healthcare across a range of medical specialties. The unmatched accuracy and precision they offer, which reduces human mistakes during crucial medical procedures, is one of their main advantages.
-
Minimally invasive surgeries can greatly reduce client trauma and hasten recovery times thanks to robotic surgical technologies.
-
Enhanced efficiency in healthcare is an additional benefit of precision medicine robotics. Robotics helps healthcare institutions maximize resource usage and enhance patient care robots throughput by optimizing workflow operations.
-
Additionally, robots are essential to the provision of remote healthcare. For example, telemedicine robots enable medical practitioners to interact with patients remotely, provide consultations, and even carry out specific medical procedures.
-
Finally, there is little doubt that automation and robotics-assisted therapy greatly improve patient safety.
Challenges in Implementing Robotics in Healthcare
AI in Healthcare, robotics-assisted therapy offers many benefits, but its successful application would require addressing several issues and concerns.
-
To begin with, money is a major consideration because robotic systems might have hefty upfront and ongoing maintenance costs.
-
Secondly, for healthcare personnel to effectively operate and incorporate robotic technologies into current medical practices, they must receive specific training.
-
Thirdly, it's critical to adhere to ethical principles and legal requirements. Strict regulatory standards must be followed by robotic systems, according to healthcare experts, to protect patient safety, confidentiality of information, and responsible utilization of technology.
-
Ultimately, the effective incorporation of robotic technology into healthcare environments depends on interoperability.
Enhancing Surgical Precision with Robotics
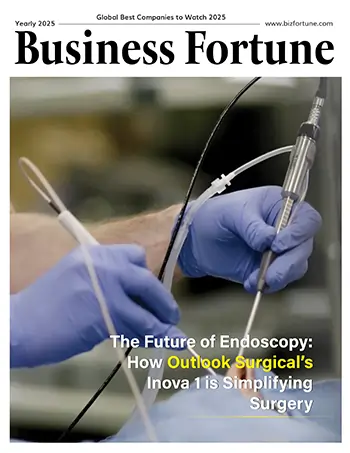
With robotic surgery, physicians may carry out a wide range of intricate treatments with greater control, precision, and flexibility than they could with conventional methods. Tiny incisions through laparoscopy are routinely used to do robotic surgery.
Improving Patient Outcomes with Medical Robots
The use of surgical robots in general healthcare is about to become more commonplace. It will provide a wider range of minimally invasive choices for different medical specializations. As robotic systems get more flexible and adaptive, they will be able to handle an expanding number of surgical operations. Less trauma, faster recuperations, and fewer incisions can all benefit patients. Surgeons now have access to precise instruments that improve their skills and surgical results.
Technical and Operational Hurdles
There are hazards associated with robotic surgery, some of which may be comparable to those associated with open surgery in the past, such as a slight chance of infection along with additional consequences.
However, surgeons who employ the robotic system discover that it can improve control, flexibility, and precision throughout the procedure. When compared to conventional surgical techniques, surgical robots technology also improves the visibility of the operating site. Surgeons can carry out intricate and delicate treatments with robotic surgery that would be challenging or impossible to accomplish with other techniques.
The Role of Telemedicine Robots in Remote Care
It has been discovered that telemedicine robots has several advantages over traditional, in-person medical interactions for patients as well as healthcare providers. These advantages include reduced travel expenses and time, fewer hours spent in waiting areas, a lower chance of communicable disease transmission, a shorter total encounter duration, more convenience, and more.
Efficiency Gains from Healthcare Automation
AI in Healthcare automation industry, workflow automation lessens manual and repetitive activities for physicians and other medical staff, reducing administrative burden and preventing stress and burnout at work.
Addressing Ethical and Privacy Concerns
Nearly every element of our daily life is impacted by technology. We use mobile and electronic modes to connect and are getting more at ease with sharing and receiving data regarding our personal and work lives.
- The Physician-Patient Interaction
The therapeutic benefit of the in-person clinic contact is one of the long-standing tenets of the doctor-patient relationship. Physicians' emphases on a thorough history and physical examination, as well as the current reimbursement schemes, are indicative of this. As medical professionals, we are taught the value of relationships between patients and doctors as the cornerstone for developing empathy and mutual trust. Guidelines also reflect this norm.
- Risks to Patient Confidentiality
Privacy is a genuine concern. It's possible for patients to be unaware of precisely who will be handling and disclosing their private medical information. The fact that the data is accessible from various computers and devices raises the risk of security lapses, which could make patients less receptive to telemedicine.
Efficiency Gains from Healthcare Automation
Through the reduction of manual labor expenses, waste minimization, workflow efficiency optimization, and the avoidance of expensive errors or delays, automation in healthcare helps healthcare organizations save money and maximize their use of resources.
Cost and Accessibility Issues in Robotics-Enhanced Care
The multiple departments at Temple University Hospital (TUH), Pennsylvania, US completed 696 robotic procedures in total in FY15, with an average of 58 cases per month. Thoracic surgery had the biggest net margin (NM), despite cardiovascular surgery having the highest contribution margin (CM). The primarily outpatient urology service had a negative NM in FY15 while possessing the highest volume & a positive CM. When 208 of the 589 robotic treatments were compared to a similar set of inpatients who underwent open procedures using the case mix index (CMI) adjustment, the mean direct cost of non-robotic operations was $6,239, which was 9% cheaper than the mean direct cost of robotic procedures. Just 3.64% ($435) less was spent on non-robotic treatments on average overall than on robotic surgeries ($11,502 vs. $11,937).
The robotic group had a reduced predicted length of stay (LOS) in comparison to the non-robotic group, which had a higher LOS, according to the UHC. For the robotic operations, the mean total direct expenses were $3,510 lower ($16,502 vs. $20,012). The duration of remain, conversion rate, transfusions rate, complications following surgery, and OR time all compared well to comparable instances reported to the STS in FY 2015. The potential cost reductions, based on data that has been published, are estimated to be between $1 and $2 million when compared to open or standard endoscopic operations that have been submitted to the STS.
Conclusion:
In conclusion, robotics is radically altering the healthcare industry. These innovations make treatments more secure and less intrusive for patients while also assisting physicians in giving better, more focused care. Not only are surgeries and monitoring of patients becoming better thanks to robots, but remote healthcare is also becoming easier and more effective.
But there are obstacles to overcome, like exorbitant expenses, the requirement for specialized instruction, and protecting patient privacy. It's critical to pay attention to these concerns as robotics becomes more and more integrated into healthcare to reap the full benefits of this technology. With the aid of robots, the future of healthcare appears bright, opening the door for better patient outcomes and care.
FAQ:
- How does robotics enhance surgical precision?
By using sophisticated robotic tools and making few incisions, sophisticated treatments can be carried out by surgeons with increased control and precision.
- What are the key benefits of using medical robots in healthcare?
Better surgical results, shorter recuperation periods, more productive workflows, and the capacity to offer remote consultations are a few examples.
- How do telemedicine robots contribute to remote patient care?
Through making it possible for virtual consultations, lowering the need for travel, and facilitating safer and more convenient patient-provider interactions.
- What challenges are associated with implementing robotics in healthcare?
Incorporate exorbitant expenses, the requirement for personnel to undergo specialized training, guaranteeing adherence to rules and regulations, and preserving compatibility with current systems.